OPIOID ADDICTION
Listen to the audio version of this article:
Cravings are one of the primary 11 symptoms of any addiction, hence they deserve our attention in treatment. We need to help you manage cravings to help prevent relapse. There are different strategies to clinically manage cravings, some through medication approaches and some through therapy techniques and coping skills.
A craving is a burning drive to use a substance. It is more than a thought to use and is initiated out of your consciousness. Cravings often feel as if life itself is dependent on taking the substance. This is not simply the power of ‘craving chocolate.’ People will go to extreme lengths to acquire drugs or alcohol when experiencing heavy cravings.
How Long do They Last?
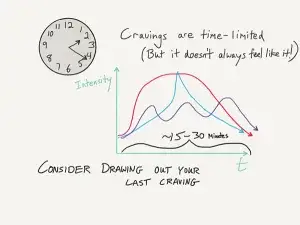
There are many different reports of how long cravings last, so this seems to be person-specific. Some people will describe them always subsiding by 20 minutes. Other reports have them lingering for up to 2 hours. Ultimately, cravings are time-limited and will subside when given enough time, so much of the management strategies employ distraction components.
Imaging studies have shown that dopamine is highly linked to cravings in the brain. Specifically looking at cocaine addiction, there is clinical evidence that the brain will ‘light up’ with neuro-activity when exposed to cues such as drug paraphernalia. By using medications that impact dopamine in the brain, it is possible to modulate cravings to some extent. The role of dopamine in addiction is crucial, and distortions in dopamine pathways can lead to continued drug use. For opioid, alcohol and nicotine addictions, we have strong medications that decrease cravings and we can use those meds along with coping skills approaches to treat your cravings.
Medication-Assisted Treatment (MAT) for Opioid Cravings
A common finding from clinical studies that researched buprenorphine was its efficacy at reducing cravings. The partial-opioid quality of buprenorphine seems to satisfy this burning desire of the brain such that cravings tend to be minimal. If you have strong cravings during buprenorphine maintenance, talk to your doctor about increasing your maintenance dose. We will often prescribe a maintenance dose up to a maximum of 16mg daily until cravings are well managed. There is some data that doses of buprenorphine greater than 16mg per day offer diminishing returns for craving reduction, so you may get a targeted 16mg dose.
Abstinence medications such as injectable naltrexone also seem to reduce cravings, but this may be through a different mechanism. The naltrexone medication does not technically ‘satisfy’ the opioid center in the brain as does buprenorphine. Instead, there is something psychological occurring. When a person is ‘blocked out’ from using opioids and does not really have access, cravings tend to subside. The inverse of this is also true. If an alcoholic buys a tavern and spends a lot of time around alcohol, cravings to drink can be so strong that the person just caves and relapses. We care about substance access in early recovery.
Alcoholism Approaches using MAT
The most studied medication shown to reduce cravings to drink alcohol is naltrexone. Even though this medication was initially developed to prevent opioid use, it has shown through numerous research studies its efficacy for alcoholism. The mechanism for this is not entirely understood. Because alcohol activates a few different neurological pathways in the brain, we know scientifically that the opioid and pain pathway is also involved. Through blocking activity in the opioid receptor via naltrexone, feedback loops that cause cravings to drink diminished.
Other medications that have been shown to be helpful in reducing alcoholism cravings include glutamate modulators. These include such meds as gabapentin and topiramate. Interestingly, these are also anti-seizure medications. Through helping the nervous system effectively calm down, the individual reports fewer cravings to drink. Of note, these medications are considered off-label approaches to treat alcoholism, whereas naltrexone is FDA approved to treat alcoholism.
MAT for Nicotine Cravings
Medication can be used to help prevent relapse on tobacco products. Nicotine replacement products such as patches or gum can be used to help treat withdrawal symptoms and to alleviate strong cravings to smoke. Other medications such as bupropion and varenicline have very good data supporting their use in tobacco cessation. In fact, the statistical numbers for these medication approaches show success rates between 63 and 71%.
If you are making an attempt to quit tobacco, talk to your doctor about the medication options. The strong efficacy of these approaches shows that they are very useful tools and should be used strategically to help boost your efforts.
Coping Skills for Cravings
There are many different coping skills to learn to improve your recovery. Skills used to cope with cravings are divided into three different categories:
- Distraction techniques
- Talking skills (Either talking with others or ‘self talk’)
- Urge surfing
Distraction Techniques
It is important to remember that cravings can be extremely powerful, but don’t last forever. Many people will report that cravings last 20 minutes or less. This is especially important when we’re talking about distraction as a useful technique. By occupying your brain with a focused activity, the mental energy devoted to the craving is taken away. Good examples of distraction include:
- Listening to music
- Going for a walk or other brief exercise
- Eating a snack
- Reading a magazine article
Talking Skills
We break talking into two categories: Talking with others and Self-Talk. Each involves moving the unconscious process of craving to something much more conscious. This is analogous to bringing the skeleton out of the closet and into the light (cravings and addiction love the darkness…).
Communication prevents you from being ‘blind-sided’ by the cravings and potential drug use. Even if you are talking to yourself, you can self-validate that the cravings are normal and won’t last forever. Here is a quick script of how this can go:
- You: I’m really struggling here! I don’t even know if I can do this anymore. These cravings just burn at me…
- Listener: I get it. What do you need? Is there anything I can do to help you out? You aren’t fighting alone anymore!
- You: Thanks for just sitting with me. That helps more than you’d think!
Urge Surfing
This coping skill is the most abstract of the three, in that it embraces some mindfulness techniques. It is a little different than distraction skills based on how it feels. You start feeling agitated and then gradually feel grounded and more physically centered. The mindful ingredients include staying very present with how you feel, avoiding judgments about your thoughts and emotions, and essentially remaining ‘still.’
This concept of being ‘still’ is also abstract, in that you can urge surf while staying physically active, such as riding your bike. It instead means that you are very much accepting the craving symptom without a drive to change it. Interestingly, the more you let go of the craving and accept what it is, the less power it will have over you and the sooner it will leave.
The mental imagery used for urge surfing often can involve water such as an actual wave crashing into the shore or a stream flowing past. You might visualize the power of the stream and feel the acceptance that you can’t actually put pressure to stop the powerful energy. You instead trust that the craving will be washed out of sight with time. This technique emphasizes patience and the peace that the craving will subside on its own.
Final Thoughts
Helping people to understand cravings as a normal part of the recovery process is needed to fully heal from addiction. We can use some medication approaches to help, and this depends on which form of addiction you experience. Learning effective coping skills is always valuable and can be used for cravings for any and all forms of addiction.
Read more CeDAR Education Articles about Opioid Addiction including Harm Reduction.
