ADDICTION SCIENCE
It is more expected that people will experience a relapse on their substance than an exception. This seems to be connected to multiple factors including the pervasive behaviors present with an addiction, the difficulty to build permanent change, and the genetic vulnerability that people with addiction carry.
Many people experience significant remorse and shame about experiencing an addiction relapse. This shame can be described as a sense of failure, or as what the author Brene Brown would describe, “Fear of being cast out from the group.” It is common that people through their recovery will become tighter with a group of peers or their family. Through the relapse, they would feel that they have failed the group or their loved ones.
Deal with the Setback
It would be incorrect to ignore the pain present in a relapse and to simply say “no problem.” Our goal through recovery is to help you maintain a commitment to your health. Relapses often are unhealthy setbacks. We need to acknowledge the setback and process this first. In working with people in treatment, we would look at a few things, namely:
- Dropout from Treatment
- Severe Life Stressors
- Poor Lifestyle Management (abandoning exercise, diet, meditation, hobbies)
- Lack of Disease Acceptance
Through pondering some of these clinical questions, you gain greater insight into the relapse and help protect yourself moving forward. It is also very possible that there is no good explanation for a relapse. This would connect very closely to a chronic disease model of addiction which acknowledges that relapse is an inherent part of the disease cycle.
What are the Goals?
We can always look at secondary and primary goals through this process. The secondary goal always is the sobriety itself; the primary goal is treatment retention. In this way, the person has an adequate buffer and built-in supportive network to help amidst the relapse. Using that network helps someone stabilize quickly before the relapse becomes too overwhelming or toxic.
If there is no built-in recovery infrastructure, a relapse can go on for many months and progress back to severe life or health consequences, a return to tolerance and inevitable withdrawal from the substance, and worsened trust in a family system. We wish to avoid all of these things, and a therapeutic connection makes all the difference.
Do you need Outpatient Counseling?
Rehabilitative Relationships
Remember the options for rehabilitative relationships, as you may need to revisit this if you struggle with a relapse and realize you have significantly distanced from your support system.
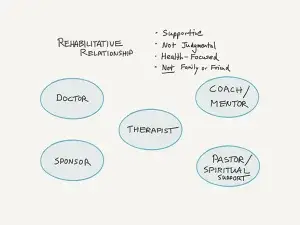
If you distanced from one of these relationships, we would need to problem solve that. What are some examples of why someone may distance?
- Financial limitations in seeing a private therapist
- Moving away – either you or your sponsor moves
- An interpersonal conflict with the relationship
- “Life got in the way”
- Unconscious preparation for relapse through cravings
The concept of unconscious, premeditated addiction relapse is fascinating. Through our care at CeDAR, we would say that a relapse “occurs” many weeks or months before the drinking or drug use. This speaks to the deeper connections (or lack of connections) in your recovery program. If this happens, it is the most important therapeutic hurdle for you to address. Why did that distance happen and would you be willing to re-engage?
The Dialectical Approach
A dialectic involves two mutually exclusive truths that co-exist. We can use this in many forms of therapy and to describe complex relationships. It is especially useful in the relapse paradigm. Through this we emphasize the co-existence of the following statements:
Relapses are part of the addiction disease
and
DON’T RELAPSE
Another way of thinking through this is the concept of a cold and yet warm approach. Supportive yet firm about our goals. Too passive prevents motivation to succeed and grow. Too judgmental prevents self-empathy and hope.
Final Thoughts
In tying together much of the chronic disease literature for addiction recovery, there always seems to be an emphasis on maintaining the therapeutic dialogue. Keeping that dialogue going is analogous to continuing to see your endocrinologist if you have diabetes. You wouldn’t simply drop out – you’d schedule some follow-up appointments and work collaboratively. The same is true for addiction recovery engagement. Through that engagement, you are better prepared to handle the crisis of a relapse, problem solve, and regroup. If the dialogue has extinguished over time, it can seem too overwhelming to reconnect with treatment.
The Dialogue Must Live!
Through the dialogue, you are able to stay curious, problem-solve, garner support, and stay vigilant. When the dialogue burns out or goes cold, your vulnerability goes up. Hold on to someone to continue your dialogue. There are many available people to choose from and all can be helpful. At CeDAR, we offer multiple avenues for a dialogue – ongoing therapy, connections with peer support, alumni meetings, recovery coaches, volunteer options, etc. These dialogues can make a significant difference in establishing a long-term recovery commitment. Through this commitment, you’ll be able to remember what recovery is all about in the first place: HEALTH
Read more CeDAR Education Articles about Addiction Science including Post Acute Withdrawal Syndrome.
