Click here to listen to the audio version
ADDICTION SCIENCE
One of the most powerful traits of the central nervous system is that of neuroplasticity. The definition of ‘plastic’ involves a malleable or moldable nature to a compound. This is exactly what happens with the nervous system. Neuroplasticity involves the brain adapting and growing to maintain a sense of homeostasis, or balance, in response to environmental pressures. Some of the examples of these pressures can include:
- Substance use (Drugs and/or Alcohol)
- Medications
- Blood Pressure changes
- Stress levels
- Hormonal change
For our purposes, we’ll discuss some of the neurologic changes taking place in the brain secondary to continuous substance use. There is good clinical data, including neuroimaging data, that shows neuroplasticity occurring in the structure and function of the brain. This includes changes in the way the brain handles the most important neurotransmitter involved in addiction – dopamine.
Dopamine is a neurotransmitter synthesized from amino acids, specifically from phenylalanine. Dietary sources initially introduce this amino acid, which then metabolizes by numerous channels to form dopamine. Dopamine is also broken down by other enzymes in a cyclical fashion, with the final product being homovanillic acid.
Dopamine serves multiple purposes in the brain including involvement in motor control, mood, and reward processing. This reward component of dopamine is the primary reason we care about this chemical in the field of addiction.
Feedback Loops and the Prefrontal Cortex
One of the largest neuro-imaging breakthroughs in addiction science was found by Nora Volkow, MD. She determined that chronic cocaine ingestion would lead to increased dopamine activity in the nucleus accumbens and ventral tegmental area (deep brain areas of the thalamus). She also found that the dorsolateral prefrontal cortex (the front part of the brain), showed dopamine desensitization. This essentially meant that the addictive ‘circuit’ in the brain became hyperactive. Becoming less responsive was the executive function zone, or ‘brake package’ if you will.
See citing of her full analysis of this and summary of some of her clinical work in her article:
- Volkow, Nora D., George F. Koob, and A. Thomas McLellan. “Neurobiologic advances from the brain disease model of addiction.” New England Journal of Medicine 374.4 (2016): 363-371.
If a person has an overactive driving force in combination with a decreased ability to regulate and say ‘no,’ what may have started as habitual drug use progresses to compulsive drug use. This evidence furthers our understanding of addiction as a disease process with neurobiological change occurring through plasticity.
Neuroplasticity Connected to ADHD
Attention-Deficit Hyperactivity Disorder (ADHD) seems to have a similar presentation in terms of the prefrontal cortex. People diagnosed with ADHD who have struggled since birth also show markedly diminished dopamine activity in this area. They regularly report associated difficulties with impulse control, organization, and mood regulation. As you could imagine, young adults and teens with substance abuse issues have as high as a 50% rate of co-occurring ADHD.
This can become a magnified problem for certain people. They have the core biology of ADHD, associated impulse control deficits, drug use in a repetitive fashion leading to habituation, and resultant down-regulation of the prefrontal cortex. This person then develops further difficulties with impulse control, more drug use, etc. ADHD is a significant risk factor for addiction and ongoing addiction makes some people appear like someone with ADHD.
By understanding the adaptation of the brain connected to substance use, we can be more understanding of impulse control issues with addicted people. We also can use this information to address a potential diagnosis of ADHD. A licensed medical professional will diagnose ADHD in people through rigorous evaluations, as ADHD can be over-diagnosed in the addicted population. Doctors may use performance testing and other advanced screening measures to make the diagnosis. It is possible to help a person heal from both substance use and ADHD conditions if the emphasis is directed toward safety, the need for clean and stable recovery time, and accurate diagnostic assessment.
Tying Things Together
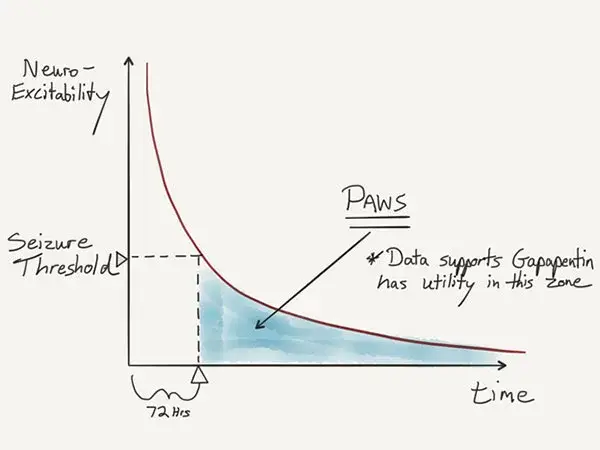
Understanding the early neurobiology of recovery is incredibly important for both clinicians and people because this period of time often includes emotional distress, personal crisis through unemployment or family breakdown, and ambivalence regarding treatment retention. An appreciation for PAWS can help validate the distress as a disease state deserving attention, rather than a discontented behavioral state. If we can alleviate some of these symptoms, the person feels more comfortable and is more likely to stay engaged in treatment.
Qualified clinicians will make an effort to screen for co-occurring ADHD, as this can compound the PAWS presentation and make relapse prevention more difficult. In these cases, we try to be thorough and evidence-based around the diagnosis. because treatment options can have potential side effects and consequences. We work to deliver a dual-diagnosis treatment plan for these people.
High-level treatment facilities will also use diagnostic assessments to make clinical recommendations. Early recovery can be highly dangerous for someone with significant neuro-excitability and/or ADHD. Much of structured addiction treatment help people during this early, vulnerable period. Accurately identifying issues and providing the right level of treatment is vital to help people stabilize and progress to a long-term recovery experience.