OPIOID ADDICTION
Listen to the audio version of this article:
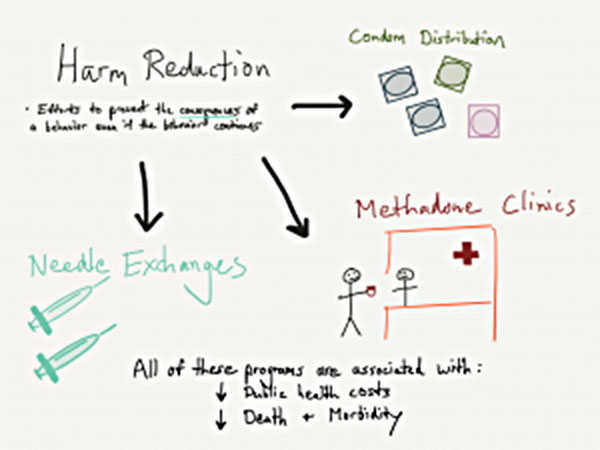
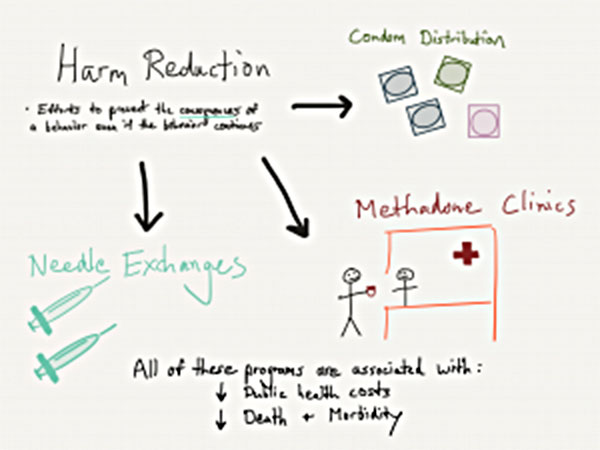
Interestingly, not all of the work in addiction treatment focuses on helping people get off and stay off drugs. There is considerable effort to target health as a whole. It does involve interventions to help those struggling with addiction who are ambivalent or even opposed to quitting. This brings us to the topic of harm reduction.
Harm reduction involves using programs or strategies to help decrease health consequences of drug use even if drug use continues. Some of this involves efforts to help preserve as much overall health as possible with the assumption that the individual will at some point reach a stage of change to quit drugs, but isn’t quite ready yet. It is in the person’s (and the public’s) best interest to decrease mortality from drugs, decrease rates of severe infections such as Hepatitis C or HIV, and decrease legal harm connected to the drug trade.
Some of the core examples of harm reduction practices include the following.
Needle Exchanges
A needle exchange involves a safe zone, typically in larger urban centers, where intravenous drug users dispose of used drug needles. They then receive packages of clean ones. These programs often have compacts built with the local police department to minimize police traffic around the center. This is to promote the health benefits of clean needle usage without threatening addicted individuals for potential drug possession charges. Most needle exchanges offer guidance to help bridge people into treatment when they are ready.
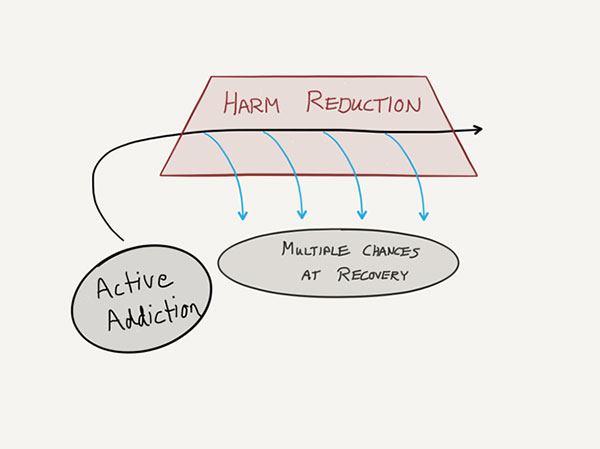
A core philosophy of needle exchanges is that the IV user will eventually reach motivation to change. We should keep a close dialogue with that person to “strike while the iron is hot.” This is rather than badger the person about their need to stop using heroin. These centers are often well-connected and have multiple referral channels to bridge a client into treatment if desired.
What are some of the data points connected to needle exchanges and public health impact? A comprehensive review by the World Health Organization in 2004 analyzed multiple domains connected to needle exchanges. Findings showed that helping addicted individuals have access to clean needles significantly reduced cases of HIV infection. They are cost-effective for communities and carried no significant unintended consequences. [1] More recent cost analysis as described by the Harm Reduction Action Center (HRAC) in Colorado reports that the cost of providing HIV care today is around $400,000 per case. That amount spent on needle exchanges would prevent an estimated 30 new HIV cases from ever contracting. [2]
Methadone
The methadone opioid replacement therapy approach is the origin of medication-assisted treatment (MAT) for opioid addiction. Cclinicians Isbell and Vogel developed this plan in New York City in 1964. It was implemented to combat the heroin crisis from post-World War II Veterans. At that time, heroin overdose was the leading cause of death for young adults in NYC. Maintenance on methadone was found to be significantly helpful in preventing opioid deaths and relapse rates. The first clinics of this sort were actively supported by the US Department of Health and the Kennedy Administration in 1963. [3]
Understanding methadone programs as harm reduction efforts can be confusing and also subject to debate. Many clinicians in dedicated methadone programs will refer to people as actively in recovery. Their primary drug of choice removed from the equation, life functioning and stability have markedly improved. The nature of methadone as a full opioid raises some controversy with certain clinicians. It implies that the brain is still receiving a close variant of its drug of choice, albeit in a less volatile way.
Methadone also carries some stigma in the dedicated 12-step recovery community. There are multiple Narcotics Anonymous meetings worldwide in which a person on methadone maintenance is not openly welcomed. These practices seem to be changing overall. This is largely as a result of the positive benefits of Buprenorphine treatment, a similar MAT approach.
Overall, methadone maintenance is associated with a statistically significant reduction in overdose deaths. It’s also credited with reducing contraction of HIV, contraction of Hepatitis C, and IV drug use as a whole.
Primary Care Harm Reduction – Condom Distribution
Another example of harm reduction, not primarily connected to addiction, is condom distribution in schools. Through efforts originating in the 1990s, increased access and education for teens to understand birth control and sexually transmitted disease (STD) prevention was effective at decreasing teen pregnancy and STD infections. Prior to these educational and distribution programs, abstinence-only approaches were not found to be effective in curbing these health issues. Of note, some of the newer data on this topic is controversial, as described in a 2016 article in The Atlantic. Data from that review showed marked shifts in teenage birth control choices with a greater emphasis on oral contraceptive approaches and varying results for teens who received condoms with or without educational efforts.
Naloxone Training and Distribution
The most recent development in harm reduction practices has been the civilian distribution of naloxone medication, the overdose antidote with brand name Narcan. In the last 5 years, more states have passed laws allowing ‘civilians’ to receive prescriptions from doctors for naloxone without the bona fide doctor-patient relationship. These laws allowed a doctor who was treating a person with a heroin problem to write a supplemental prescription to the person’s family member. The hope in this action was that if the addicted individual were found down from a heroin overdose, that family member could administer the life-saving measure that was previously only in the hands of EMTs or ER personnel.
Naloxone programs are now nation-wide and represent a public health approach to address the most tragic outcome of the opioid epidemic – overdose deaths. Numerous media articles reviewing naloxone programs and harm reduction centers seem to be promoting these on a scale in parallel to needle exchange efforts. By helping to stifle the most toxic of outcomes from opioid use, the user is able to have as much preserved time as possible to make decisions about change and quitting opioids.
How this Applies to You
If you are struggling with opioid addiction, these options for harm reduction are available to you and likely in your best interest. It is extremely important to remember that recovery efforts are possible amidst harm reduction. Don’t consider recovery efforts and harm reduction efforts as mutually exclusive, especially towards the beginning of your change process.
During the change, the body and mind are disrupted. Even though you are working to heal yourself and your addiction, there is a terrible irony that you’re overdose and mortality rate is actually heightened at this time. Opioid tolerance is decreased and the brain will respond more intensely to opioid use. This can lead to an opioid overdose as someone may resume use just as at the height of the addiction.
Residential treatment centers around the country are more assertively embracing harm reduction practices. If someone in active treatment is able to effectively detox off of opioids and has reached the 30-day recovery milestone, that person is still at 3-4 times increased the chance of death the weeks following discharge from treatment. It is for this reason that opioid-dependent people, especially IV heroin users and young adults, require structured treatment for periods longer than 30 days. A strong treatment program will appreciate the opioid overdose risk and match treatment needs appropriately.
[1] Effectiveness of sterile needle and syringe programming in reducing HIV/AIDS among injecting drug users. Evidence of Action Technical Papers. World Health Organization 2004.
[2] Fact Sheet. Harm Reduction Action Center Website. 2017 http://harmreductionactioncenter.org/fact-sheet/
[3] Methadone maintenance treatment (MMT). H Joseph, S Stancliff, J Langrod. Mount Sinai Journal of Medicine. 2000
Read more CeDAR Education Articles about Opioid Addiction including Brain Change.